The Nielson Lab has shut down and will no longer be conducting clinical research at the University of Minnesota. Dr. Nielson is retaining an adjunct appointment and will continue to publish the results from this research and create educational material for the public, and will be transitioning to more grassroots community work through the Psychedelic Society of Minnesota, and advocacy and drug policy work through the Psychedelic Medicine Task Force.
The overarching purpose of the work in the Nielson lab is to understand and treat trauma. Research projects in the lab utilizes a multidisciplinary approach, merging the fields of neurobiology, psychiatry and informatics to identify more precise "bio-types" of trauma psychopathology than traditional diagnostic criteria, and potential novel targets for treatment. We use established and emerging machine learning methods with multi-modal data spanning across a diverse range of diagnostic categories for neuropsychiatric disorders. Our approach can be used to run hypotheses on in silico models to understand the complexity involved in these disorders. An advantage of such approaches is the minimization for the need to test hypotheses in animal models (in vivo). Dr. Nielson received an Early Stage Investigator (ESI) award from NIMH to apply these methods to large datasets from trauma-exposed patients to identify and validate dimensions of post-traumatic stress (PTS), relevant biological predictors, and precision treatment response trajectories.
Other areas of focus in the Nielson lab were dedicated to psychedelic neuroscience research and drug policy reform. Dr. Nielson has collected data through several anonymous online survey to assess benefits and risks of ayahuasca use in naturalistic settings to treat symptoms of trauma, unique experiences of BIPOC psychedelic users, and documenting unique adverse events for people living with spinal cord injury who use psychedelics. Dr. Nielson also conducted the first psilocybin clinical trial at the University of Minnesota aiming to tease out the neurological mechanisms of altered states of consciousness and their role in promoting neuroplasticity and wellness in healthy research participants (NCT04424225). This work was funded by the Psychedelic-Assisted THerapy (PATH) Fund through the UMN Foundation, which was created thanks to a generous donation from the local community, as well as funding from the Heffter Research Institute Young Investigator Program. These, and other data, are part of a larger network of data supporting the potential for psychedelic therapies and experiences to promote wellness across a diverse range of mental health disorders (see network below).
Mental Health Informatics Research
Recent efforts to optimize diagnosis and treatment planning for psychiatric disorders through the Research Domain Criteria (RDoC) and ongoing clinical trials have generated large datasets housed in the NIMH Data Archive (NDA). The NDA is a valuable resource for data-driven discovery in mental health research. Data across multiple units of measure from a wide array of disorders are housed in the NDA. We mine data from the NDA, and other similar data repositories, to characterize biotypes that span across diagnostic categories, and the complex constellation of symptoms and functional deficits that can be measured in individual patients, and potential treatment targets for future research.
Results from these studies can be found on the Publications page.
Psychedelic Research
Psychedelic research is undergoing a renaissance within the scientific arena, where an astounding volume of literature and data are emerging to support this new frontier in science and medicine. There is also increasing attention being paid in the popular press towards their therapeutic potential, including notable mediums like The New Yorker, NY Times, and Rolling Stone. Additionally, compounds such as MDMA and psilocybin have recently been granted breakthrough therapy designation by the FDA for PTSD and depression, respectively, making this area of research an exciting and innovative avenue for continued scientific exploration into their mechanisms of action.
Psychedelic research in my lab focused on collecting data from completed and ongoing psychedelic research studies to develop an evidence base for drug policy reform and treatment planning, as well as to understand the mechanisms for how these compounds inform new models about information processing in the human brain. Projects include analysis of data from anonymous online surveys, including a study of ayahuasca users in naturalistic settings (see "Media" and "Publications" tabs for results), and unique perspectives of marginalized communities often excluded or not represented in clinical trials with psychedelics.
The network below is a working model of overlapping symptoms of trauma, and various psychedelic therapies that have published research (red numbers and reference list) suggesting a therapeutic benefit.
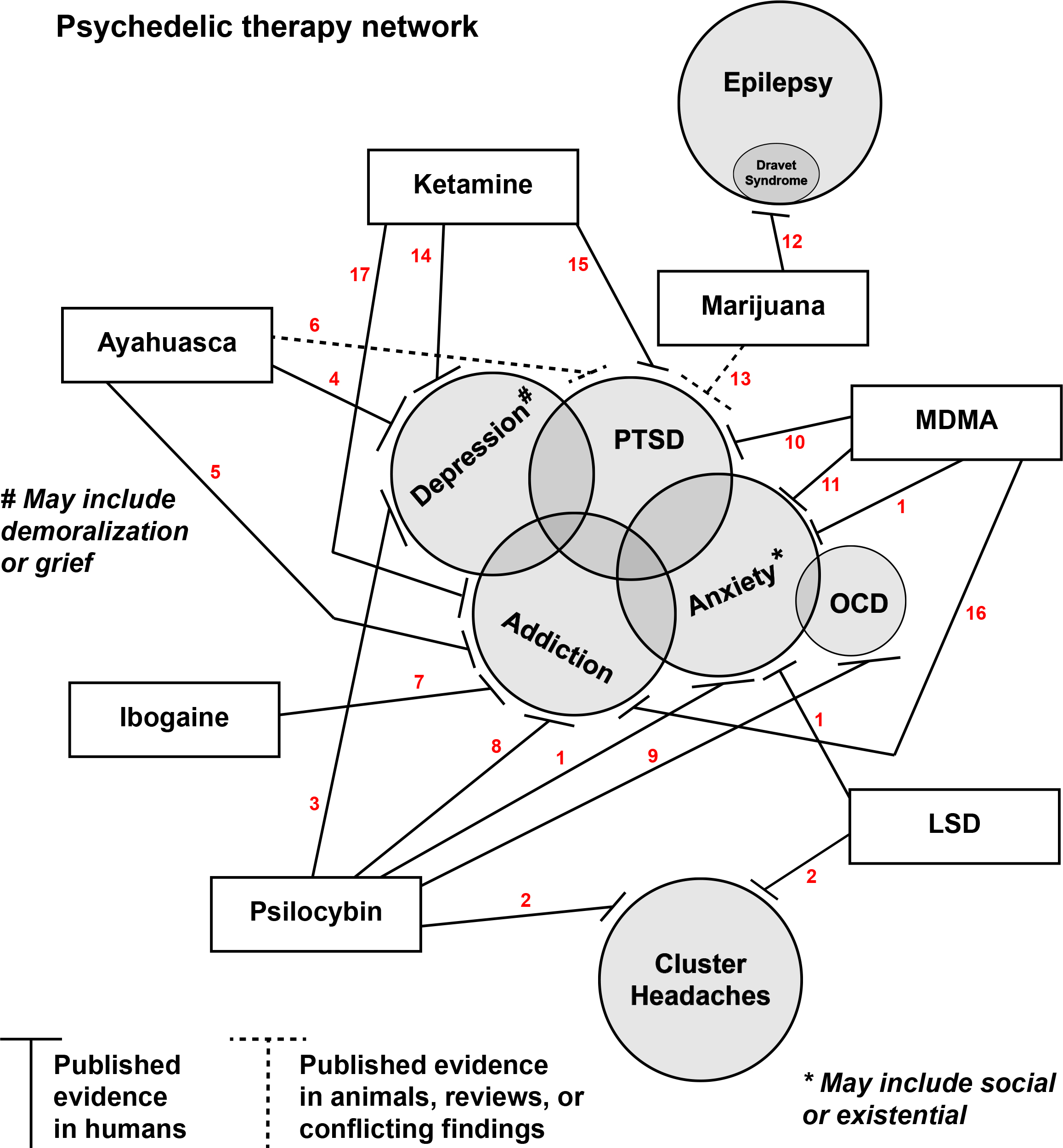
References for psychedelic therapy network
1. LSD, psilocybin or MDMA for end of life anxiety
Pilot Study of Psilocybin Treatment for Anxiety in Patients With Advanced-Stage Cancer
Individual Experiences in Four Cancer Patients Following Psilocybin-Assisted Psychotherapy
Acute and Sustained Reductions in Loss of Meaning and Suicidal Ideation Following Psilocybin-Assisted Psychotherapy for Psychiatric and Existential Distress in Life-Threatening Cancer
MDMA-assisted psychotherapy for treatment of anxiety and other psychological distress related to life-threatening illnesses: a randomized pilot study
2. LSD and psilocybin for migraine and cluster headaches
Response of cluster headache to psilocybin and LSD
Indoleamine Hallucinogens in Cluster Headache: Results of the Clusterbusters Medication Use Survey
Exploratory Controlled Study of the Migraine-Suppressing Effects of Psilocybin
3. Psilocybin for depression
Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms
Increased amygdala responses to emotional faces after psilocybin for treatment-resistant depression
Psilocybin with psychological support for treatment-resistant depression: six-month follow-up
Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial
Trial of Psilocybin versus Escitalopram for Depression
Single-Dose Psilocybin for a Treatment-Resistant Episode of Major Depression
Single-Dose Psilocybin Treatment for Major Depressive Disorder: A Randomized Clinical Trial
4. Ayahuasca for depression
Therapeutic potential of ayahuasca in grief: a prospective, observational study
5. Ayahuasca for addiction
Ayahuasca-Assisted Therapy for Addiction: Results from a Preliminary Observational Study in Canada
6. Ayahuasca for PTSD
Ayahuasca as a Candidate Therapy for PTSD
A Qualitative Assessment of Risks and Benefits of Ayahuasca for Trauma Survivors
7. Ibogaine for addiction
Ibogaine: Complex Pharmacokinetics, Concerns for Safety, and Preliminary Efficacy Measures
Noribogaine reduces nicotine self-administration in rats
Ibogaine treatment outcomes for opioid dependence from a twelve-month follow-up observational study
Treatment of opioid use disorder with ibogaine: detoxification and drug use outcomes
8. Psilocybin for addiction
Pilot Study of the 5-HT2AR Agonist Psilocybin in the Treatment of Tobacco Addiction
Psilocybin-assisted treatment for alcohol dependence: A proof-of-concept study
Psilocybin-occasioned Mystical Experiences in the Treatment of Tobacco Addiction
Long-term Follow-up of Psilocybin-facilitated Smoking Cessation
Psychedelic therapy for smoking cessation: Qualitative analysis of participant accounts
9. Psilocybin for OCD
Safety, Tolerability, and Efficacy of Psilocybin in 9 Patients With Obsessive-Compulsive Disorder
Psilocybin and Obsessive Compulsive Disorder
10. MDMA for PTSD
Posttraumatic Growth After MDMA-Assisted Psychotherapy for Posttraumatic Stress Disorder
MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study
MDMA-assisted therapy for moderate to severe PTSD: a randomized, placebo-controlled phase 3 trial
11. MDMA for social anxiety in autistic adults
MDMA-assisted therapy: A new treatment model for social anxiety in autistic adults
12. Cannabidiol for Dravet's syndrome
Cannabidiol in patients with treatment-resistant epilepsy: an open-label interventional trial
Trial of Cannabidiol for Drug-Resistant Seizures in the Dravet Syndrome
13. Marijuana for PTSD
On Disruption of Fear Memory by Reconsolidation Blockade: Evidence from Cannabidiol Treatment
Cannabidiol Regulation of Learned Fear: Implications for Treating Anxiety-Related Disorders
PTSD Symptom Reports of Patients Evaluated for the New Mexico Medical Cannabis Program
Blunted stress reactivity in chronic cannabis users
Cannabinoid modulation of corticolimbic activation to threat in trauma-exposed adults: a preliminary study
The short-term impact of 3 smoked cannabis preparations versus placebo on PTSD symptoms: A randomized cross-over clinical trial
14. Ketamine for depression (in progress, many trials on this)
15. Ketamine for PTSD
16. MDMA for addiction
17. Ketamine for addiction
Ketamine can reduce harmful drinking by pharmacologically rewriting drinking memories